Foot pain
Share on:
Plantar fasciosis
Plantar fasciosis is pain originating from the dense band of tissue called the plantar fascia that extends from the bottom of the heel bone to the base of the toes (ball of the foot).
- The connective tissue between the heel and ball of the foot may become damaged and painful.
- Pain is often worse when first bearing weight and is felt at the heel.
- Stretches, changing footwear, wearing devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses) and splints, and sometimes corticosteroid injections can help.
The plantar fascia connects the bottom of the heel bones to the ball of the foot and is involved in walking and running, giving spring to the step.
Plantar fasciosis is sometimes referred to as plantar fasciitis. However, this term is not correct. The term fasciitis means inflammation of the fascia, but plantar fasciosis is a disorder primarily of repeated stress to the fascia rather than a disorder of inflammation. Other terms used to describe plantar fasciosis include calcaneal enthesopathy and calcaneal spur syndrome (heel spur).
However, a heel spur may or may not be present. Often a small tear results from excessive strain placed on the plantar fascia. Plantar fasciosis is one of the most common causes of heel pain.
Plantar fasciosis can develop in those who have sedentary lifestyles, wear high-heeled shoes, have unusually high or low arches in the feet, or have tight calf muscles or a tight Achilles tendon (which attaches the calf muscles to the heel bone). Sedentary people are usually affected when they suddenly increase their level of activity or wear less supportive shoes.
Plantar fasciosis is also common among runners and dancers because of the increased stress on the fascia, especially if the person also has poor foot posture. The development of this painful disorder occurs more often in people whose occupations involve standing or walking on hard surfaces for prolonged periods.
Disorders that may cause or aggravate plantar fasciosis are obesity, rheumatoid arthritis, and other types of arthritis.
Plantar fasciosis symptoms
A person with plantar fasciosis may have pain anywhere along the course of the plantar fascia but most commonly where the fascia joins the bottom of the heel bone. The person often feels a great deal of pain after resting, particularly when placing weight on the foot first thing in the morning.
The pain temporarily diminishes after the person first walks but may return later in the day. It may also begin when the person walks or runs. In this case, the pain radiates from the bottom of the heel toward the toes. Some people have burning or sticking pain along the inside border of the sole of the foot when walking.
What Is a Heel Spur?
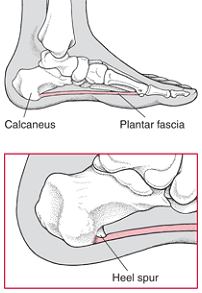
A heel spur is a growth of extra bone on the heel bone (calcaneus). It may form when the plantar fascia, the connective tissue extending from the bottom of the heel bone to the base of the toes, pulls excessively on the heel. The spur may be painful as it develops, but it may become less painful as the foot adjusts to it. Most spurs can be treated without surgery.
Heel Spur diagnosis
The doctor may make the diagnosis after examining the foot. Tenderness is evident where the plantar fascia enters the heel bone or at the bottom of the ball of the foot.
X-rays may reveal the presence of a heel spur protruding from the bottom front edge of the heel bone. This heel spur is a growth of extra bone produced over time by a combination of increased strain on the fascia and foot dysfunction.
However, people with plantar fasciosis often do not have heel spurs, and most people with heel spurs do not have pain, so the presence of heel spurs does not necessarily confirm plantar fasciosis. Other diagnostic tests, such as magnetic resonance imaging (MRI), are rarely needed.
Heel Spur treatment
To relieve the stress and pain on the fascia, the person can take shorter steps and avoid walking barefoot. Activities that involve foot impact, such as jogging, should be avoided. The person may need to lose weight. Stretching the calf muscles and foot often accelerates healing. Orthoses placed into well-fitting supportive shoes can help to cushion, elevate, and support the heel.
Other measures that may be needed include use of adhesive strapping or arch-supporting wraps, ice massage, use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as Flanax Pain Reliever Tablets, occasional corticosteroid injections into the heel, physical therapy, and splinting at night to stretch the calf muscles and fascia during sleep. Other treatments include massaging your foot with Flanax Liniment.
Corticosteroid injections should probably not be done more than a few times or else they might make the disorder worse. If these measures do not help sufficiently, a cast may be applied. If symptoms are still bothersome, surgery is very rarely required to attempt to partially release pressure on the fascia and remove any heel spurs.
Achilles tendon bursitis
Achilles tendon bursitis is inflammation of the fluid-filled sac (bursa) located either between the skin of the heel and the Achilles tendon (posterior Achilles tendon bursitis) or in front of the attachment of the Achilles tendon to the heel bone (anterior Achilles tendon bursitis, retrocalcaneal bursitis).
- Typical symptoms include swelling and warmth and a tender spot at the back of the heel.
- The diagnosis is based on symptoms, an examination, and sometimes x-rays.
- Treatment is aimed at relieving the inflammation and, depending on the location of the Achilles tendon bursitis, eliminating the pressure on the back of the heel.
The Achilles tendon is the tendon that attaches the calf muscles to the heel bone. Posterior Achilles tendon bursitis is often associated with formation of a bone prominence called Haglund's deformity or “pump bump” on the heel bone. Anterior Achilles tendon bursitis is also called Albert's disease or retromalleolar bursitis.
Posterior Achilles tendon bursitis occurs mainly in young women but can develop in men. Walking in a way that repeatedly presses the soft tissue behind the heel against the stiff back support of a shoe can cause or aggravate the bursitis. Shoes that taper sharply inward toward the posterior heel (such as high-heeled shoes) can lead to the development of this bursitis.
Bursitis in the heel
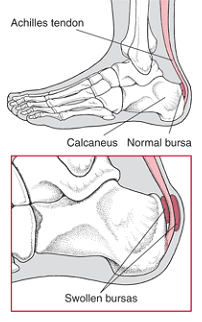
Normally, only one bursa is in the heel, between the Achilles tendon and the heel bone (calcaneus). This bursa may become inflamed, swollen, and painful, resulting in anterior Achilles tendon bursitis.
Any condition that puts extra strain on the Achilles tendon can cause anterior Achilles tendon bursitis. Injuries to the heel and diseases such as rheumatoid arthritis can also cause it.
Achilles tendon bursitis symptoms
When the bursa becomes inflamed after an injury, symptoms usually develop suddenly. When the bursa develops without an injury, symptoms may develop gradually. With both posterior and anterior Achilles tendon bursitis, symptoms usually include swelling and warmth at the back of the heel. A mildly red, swollen, tender spot develops on the back of the heel.
When the inflamed bursa enlarges, it appears as a red lump under the skin of the heel and causes pain at and above the heel. If posterior Achilles tendon bursitis becomes chronic, the swelling may become hard, fluid-filled, and red or flesh-colored.
Achilles tendon bursitis diagnosis
The diagnosis is based on the symptoms and an examination. For anterior Achilles tendon bursitis, doctors use x-rays to rule out a fracture of the heel bone or damage to the heel bone caused by rheumatoid arthritis or another inflammatory arthritis.
Achilles tendon bursitis treatment
With anterior and posterior Achilles tendon bursitis, applying warm or cool compresses to the area and using nonsteroidal anti-inflammatory drugs such as Flanax Pain Reliever Tablets can temporarily relieve the pain and inflammation. Flanax Liniment can also be applied to the affected area of the foot to relief the pain and inflammation. The Flanax Pain Reliever Tablets and Flanax Liniment can be used together to fight your foot pain.
With posterior Achilles tendon bursitis, treatment is aimed at reducing the inflammation and adjusting the foot's position in the shoe to relieve pressure and motion on the back of the heel. Foam rubber or felt heel pads can be placed in the shoe to eliminate pressure by elevating the heel. Stretching the back part of the shoe or placing padding around the inflamed bursa may help.
Sometimes a special shoe, such as a running shoe designed to stabilize the midsole heel, devices that change the position or range of movement of the foot and relieve pressure on affected joints (orthoses), or both can help to control abnormal foot and heel motion contributing to the posterior heel irritation. Other shoes have padding that reduces irritation to the posterior heel and Achilles tendon.
